Environmental Conditions
Environmental Conditions
Environmental conditions can significantly impact player health and safety. Extreme temperatures, severe weather and the integrity of the playing field and its equipment all impact players’ ability to practice and compete safely. U.S. Soccer’s Recognize to Recover program gives players, parents, coaches and referees information and guidelines to make sure the desire to play does not cloud the decision-making process when it comes to evaluating environmental conditions to ensure the safety of those on the field.

Heat & Hydration
Heat & Hydration
Extreme heat can impact players' health and safe play. Proper hydration and knowing when you need to drink are critical, to help prevent many injuries and illnesses, from muscle cramps to heat stroke. Players should drink water before, during and after a game or practice, which means coaches should make sure there is adequate water available. U.S. Soccer’s Recognize to Recover program gives players, parents, coaches and referees information and guidelines to make sure the desire to play does not cloud the decision-making process when it comes to evaluating environmental conditions to ensure the safety of those on the field.
RECOVER
- Add hydration breaks
- Shorten practice
- Practice early or late in the day when temperatures are lower
- Use less-strenuous training activities during practice
U.S. Soccer Heat Guidelines
Heat Guidelines Contributors: Korey Stringer Institute and Dr. George Chiampas
U.S. Soccer Cold Weather Guidelines
Cold Weather Guidelines Contributors: Athletico, Korey Stringer Institute and Dr. George Chiampas
RECOGNIZE
Thirst is a warning that your body is already in an early stage of dehydration. Drink when you are thirsty. Recognizing the signs of dehydration are important because the amount of water required will vary from player to player.
- Dry, sticky mouth
- Sleepiness or tiredness
- Headache
- Dizziness or lightheadedness
- Rapid heartbeat
- Rapid breathing
- Fever
- In the most serious cases, delirium or unconsciousness
Heat Guidelines
Heat Guidelines
Heat-related illnesses, such as heat stroke and heat exhaustion can be serious and potentially life-threatening conditions. U.S. Soccer’s RECOGNIZE TO RECOVER program prepared this guide for coaches, referees and players when training or playing in warmer climates, outlining recommendations for hydration breaks and participant safety during extreme temperature conditions. The information provided herein is not a substitute for medical or professional care, and you should not use the information in place of a visit, consultation or the advice of your physician or other healthcare provider. For specific questions and concerns, please consult your healthcare provider or physician.
HEAT-RELATED ILLNESS
Heat-related illnesses, such as heat exhaustion and exertional heat stroke (EHS), can be serious and potentially life-threatening conditions which can be brought on or intensified by physical activity. Recognizing the signs and symptoms as early as possible allows for treatment and rapid recovery with hydration and cooling down the individual.
• Early signs and symptoms of heat illness include weakness or fatigue, headache, nausea and dizziness
• Altered mental status, such as confusion, irritability, aggressive behavior, dizziness
• Slurred speech
• Hallucinations
• Loss of balance, falling down
• Throbbing headache
• Body temperature above 104 degrees Fahrenheit
• Complaining of chills, while skin may be warm to the touch
Preventing heat related illness is the best medicine. It may become important to adjust training, match play and hydration breaks when playing in warmer climates and during extreme temperature conditions.
• Develop and implement a heat policy (heat acclimatization guidelines, activity modification guidelines based on environmental conditions and management of heat-related illness) as part of your emergency action plan (EAP)
• Frequently monitor environmental conditions using Wet Bulb Globe Temperature (WBGT) device or Heat Index and make practice modifications (e.g., increase in the number and duration of hydration breaks, shortening practice, postponing practice/competition until cooler parts of the day)
• Follow heat acclimatization guidelines (below) during preseason practices and conditioning
• Ensure appropriate hydration policies are in place with athletes having unlimited access to water during practice and competition, especially in warm climates.
• Educate staff on the signs and symptoms of heat related illness and early management
• Consider having a health care provider such as an athletic trainer onsite for all practices and competitions
To assist coaches and athletes in this, RECOGNIZE to RECOVER created an easy reference poster. The guidelines are intended to help evaluate situations to prevent heat-related illness before it begins. The three-step Heat Guidelines include methods for evaluating danger levels and appropriate responses to those various levels
It is recommended to include scheduled hydration breaks when the WBGT reaches 89.6°F. Provide hydration breaks of four minutes for each 30 minutes of continuous play. In a regulation 90-minute match, this would schedule the hydration break at minute 30 and 75.
Provide adequate communication of environmental conditions, cooling methods and other resources to players and staff. This includes ensuring unlimited access to water and other fluids, making sure players and coaches are aware of planned breaks for hydration and the duration and time of training.
EXCESSIVE HEAT IMPACT ON PLAY
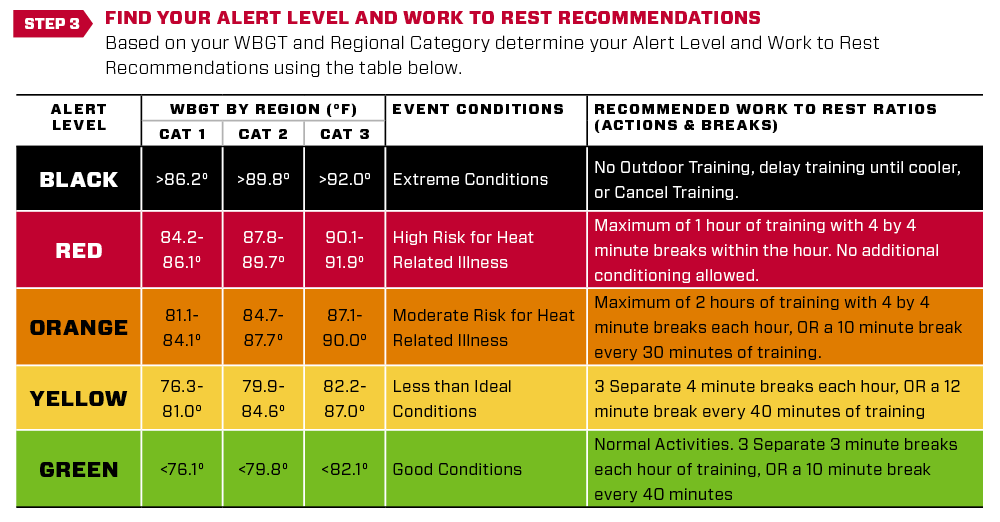
Depending on your Region Category, it is recommended that training or match play be canceled or delayed until cooler when WBGT exceeds these levels:
• Region Category 1 >86.2°F;
• Region Category 2 >89.9°F
• Region Category 3 >92.0°F
Once an alert level is determined, follow these “Work to Rest” ratios to modify training to help ensure safe play:
• Alert Level Black – No outdoor training, delay training until cooler or cancel.
• Alert Level Red – Maximum of one hour of training with four separate 4 minute breaks within the hour. No additional conditioning allowed.
• Alert Level Orange – Maximum two hours of training time with four separate 4 minute breaks each hour, or a 10 minute break after 30 minutes of continuous training
• Alert Level Yellow – Use discretion, provide three separate 4 minute breaks each hour, or a 12 minute break every 40 minutes of continuous training
• Alert Level Green – Normal Activities, provide three separate 3 minute breaks each hour of training, or a 10 minute break every 40 minutes.
HEAT POLICY
A heat policy is intended to serve as a guide for regulating match play, practice sessions, hydration breaks and participant safety during extreme temperature conditions. Such a heat policy can be shared with participants, making sure everyone is aware of the safety precautions in place. The steps listed below should be considered when developing a heat policy:
• Cool in a shaded area using ice towels, cooling tub or wading pool
• Provide access to fluids/electrolytes and encourage rehydration
• If emergency continues, call 9-1-1 for immediate medical assistance
• Ensure appropriate hydration policies are in place with athletes having unlimited access to water during practice and competition, especially in warm climates.
• Educate staff on the signs and symptoms of heat related illness and early management
• Consider having a healthcare provider such as an athletic trainer onsite for all practices and competitions
• Heat policy should be part of an overall EAP
• Prevention
• Follow heat acclimatization guidelines (see box)
• Activity modification guidelines based on environmental conditions
• Frequently monitor environmental conditions
• WBGT device or Heat Index
• Increase the number and duration of hydration breaks
• Shorten practice/reduce intensity of exercises
• Postponing practice/competition until cooler parts of the day
• Management and treatment of heat-related illness
• Remove from training and source of heat
Acclimatization
Acclimatization is the body’s natural adaptation to exercising in the heat. This process typically takes 10-14 days. Effective acclimatization should require a gradual graded progression of exercise in the heat. This typically applies at the start of preseason (summer months) where athletes are beginning fitness training and progressive training exposure in heat is recommended
GUIDE FOR ACCLIMATIZATION (10-14 DAYS)
Avoid the hottest part of the day for training sessions (11am-4pm)
Days 1-5
• One formal practice a day
• Maximum three hours of training time (this includes warm up, stretches and cool down)
Days 6-14
• Double practice days can begin day 6 and not exceed five hours in total practice time between the two practices.
• Minimum of three-hour rest period between each training session during double practice days. The three-hour rest period should be in a cool environment to allow the body to fully recover.
• Each double practice day should be followed by a single practice day with practice time not to exceed three hours.
• Athletes should receive one day rest following six days of continuous practice.
In severe cases of exertional heat stroke:
• Remove excess clothing/equipment and immediately begin cooling the athlete by placing them in an ice-water tub
• If no tub is present, rotate cold, wet ice towels every 2-3 minutes over the entire surface of the body or as much as possible
• Call 9-1-1 – Exertional heat stroke is a medical emergency
RECOVERY
• Remove from training and away from the source of heat
• Cool in a shaded area using ice towels
• Fan or spray with water to bring down body temperature
• Provide access to fluids/electrolytes and encourage rehydration
SPECIFIC HEAT-RELATED ILLNESS
The first steps to recovery in all these cases are replacing fluids and cooling the body by resting in a cool, shaded place. Fanning or spraying with water will also help bring down the body temperature.
Heat Exhaustion
Heat exhaustion is the body’s response to an excessive loss of water and salt, usually through excessive sweating. Someone suffering from heat exhaustion may appear confused or disoriented. It can lead to extreme weakness or fatigue, dizziness and nausea.
Heat Cramps
Heat cramps usually affect those who sweat a lot during strenuous activity. This sweating depletes the body’s salt level, as well as hydration. Low salt levels lead to painful muscle cramps. Heat cramps may also be a symptom of heat exhaustion.
Heat Stroke
Heat stroke is the most serious heat-related disorder. It occurs when the body becomes unable to control its temperature. When this happens, the body’s temperature rises rapidly, the sweating mechanism fails and the body is unable to cool down. The surge in body temperature can happen very quickly, within 10 to 15 minutes, rising to 106° Fahrenheit or higher. Heat stroke can cause death or permanent disability if emergency treatment is not given.
Someone suffering heat stroke will be dizzy and confused. They may slur their speech, have hallucinations or complain of a throbbing headache. While their skin may be warm to the touch, they may actually complain of chills. If you suspect heat stroke, get the on-site medical provider or call 9-1-1.
MANAGEMENT
HEat Illness (Heat Exhaustion, Heat Cramps)
• Remove from training and source of heat
• Cool in a shaded area using ice towels
• Provide access to fluids/electrolytes and encourage rehydration
Exertional Heat Stroke
• Is a medical emergency
• Immediately call EMS (911) and prepare hospital for heat related emergency
• Athlete may have confusion or altered mental status and a rectal temperature >104°F
• Remove excess clothing/equipment and immediately begin cooling the athlete by placing them in an ice-water-tub
• If no tub is present, rotate cold wet ice towels (every 2-3 minutes over the entire surface of the body or as much as possible)
AIR QUALITY INDEX GUIDELINES
AIR QUALITY INDEX GUIDELINES
If teams are aware of a potential air quality issue in their home market in advance of hosting a match, they must notify the league as soon as they become aware of the issue. Teams are to use www.AIRNOW.gov to determine AQI in the local market. AQI is to be read 1 hour prior to teams starting warmups.
Based on the reading the following must be implemented:
AQI 100-150:
Add one hydration break per half to be taken at the 30’ and 75’ or at a natural break close to the times.
Players with underlying health conditions should use caution and will communicate with local CMO and each team to monitor players with complicating health issues. To make decisions in the players best interests and risk category
EMS to have oxygen available as needed on game day-consider oxygen availability at each bench
AQI >150:
Four hydration breaks will be taken at the 15’, 30’, 60’, and 75’ or at a natural break close to the times.
Oxygen behind the benches to be supplied by teams with at least 2 masks available
Team docs start communicating regarding any at-risk players and how to best continue forward for the health of the players
Should coordinate with local public health officials and be in line with local and or regional restrictions if in place- this should take into account players and spectators
AQI approaching 180-200:
Consideration for postponing or canceling with on the ground assessment with the medical team
Should coordinate with local public health officials and be in line with local and or regional restrictions if in place- this should take into account players and spectators
AQI over 200:
Cancel or postpone
Sun Safety Guidelines
U.S. Soccer Sun Safety Guidelines
Sun Safety Guidelines
U.S. Soccer Sun Safety Guidelines
FACT
One in five adults in the U.S. will develop some form of skin cancer (1). The sun we get as children, teenagers, and young adults impacts individual risk. Prolonged sun exposure sustained while engaged in athletic endeavors is no less damaging than the ultraviolet exposure sustained at the pool, beach or in a tanning bed. Sun prevention makes a difference in reducing risk (2, 3). U.S. Soccer is committed to educating participants, coaches and referees about sunscreen use and sun prevention measures. Join U.S. Soccer in achieving this GOAL!
SUN SAFETY GUIDELINES
Use a broad spectrum, water resistant (UVA/UVB) sunscreen with an SPF of 30 or higher. Physical sunscreens with Zinc or titanium dioxide are particularly effective (4).
One ounce of sunscreen (two tablespoons) is typically needed to provide adequate coverage to the face, ears, neck, arms and legs (4).
All participants should apply sunscreen 15 minutes prior to playing soccer. Coaches and parents need to assist younger players to ensure proper application
Reapplication is necessary at least every two hours for prolonged outdoor exposure or with heavy perspiration (5)
Ultraviolet exposure occurs even on overcast days.
Check local UV index to assess risk. This index is listed on displayed on weather applications such as weather.com or accuweather. The potential for UV damage rises as UV index rises (5).
Between games and with breaks in training, seek the shade.
Cover up clothing, clothing with ultraviolet protective factor (UPF) >30, hats and UV-blocking sunglasses provide valuable additional protection
1. CDC.gov/cancer/skin/call_to_action/index.htm
2. Williams, ML and Pennella, R. Melanoma. Melanocytic nevi and other melanoma risk factors in children. J Pediatrics. 124(6): 833-845, June 1994
3. Ally, MS, Swettler, SM et al. J Amer Acad Dermatol. 78(2): 289-292, Feb 2018
4. Quatrano, NA and Dinulos. Principles of Sunscreen Use in Children. Curr Opinions in Pediatrics. 25(1): 122-129, Feb 2013
5. EPA.gov/sunsafety/UV-index-1
U.S. SOCCER RECOMMENDS THAT MATCH OFFICIALS PRACTICE THE FOLLOWING SKIN CARE GUIDELINES:
Consider wearing sun screen daily on areas of exposed skin
Apply skin protection factor (SPF) of 30 or greater 15 minutes prior to sun exposure
At a minimum, reapply every 2 hours or more frequently if sweating extensively
Take advantage of halftime to reapply
Consider wearing long sleeves (or UV protective clothing), if applicable, during high sun exposure periods
Periodically (once a year) review exposed skin for any changes or growths and consult your doctor or dermatologist
Cold Weather Guidelines
Cold Weather Guidelines
The effects of cold weather can impact health and safety during practices and games. The definition of “cold stress” varies across the United States, depending on how accustomed people are to cold weather. A player from Minnesota will have a much different threshold for cold than a player from Florida.
U.S. Soccer’s RECOGNIZE TO RECOVER program prepared this guide for coaches, referees and players for training or playing in colder climates. Additionally, it serves as a guide for match play and participant safety during extreme temperature conditions. The information provided is not a substitute for medical or professional care, and you should not use the information in place of a visit, consultation or the advice of your physician or other healthcare provider. For specific questions and concerns, please consult your health care provider or physician.
COLD WEATHER SAFETY TIPS
Stay Dry
Wet and damp conditions add to the risk of injury or illness during cold weather. Players, coaches and referees should recognize these factors and use additional caution to watch for potential cold injuries.
If players do get wet during training or play, remove wet or saturated clothing and replace it with dry clothing. This becomes more important if the individual will remain out of play or anticipates standing around for a prolonged period of time. A hat, gloves and extra pair of socks can also keep extremities dry in case of snow or rain.
Dress for the Cold
When temperatures drop and wind increases, the body loses heat more rapidly. It is important to dress appropriately when training or playing in cold weather. This also means to not overdress.
Layering clothing in a specific way (see box) is recommended and very effective. The layers can be added or removed based on body temperature and changing environmental conditions, such as temperature and wind. Allow players to wear additional clothing, like gloves, sweatshirts, sweat pants and/or hats or headbands. Also, avoid sweating before going outside because your body will cool too quickly.
Wind Chill
Pay attention to the wind chill temperature (WCT) Index. (see chart below) Even prolonged exposure in relatively mild temperatures can lead to frostbite. The National Weather Service wind chill chart can serve as a guide to safe play in cold weather.
Stay Hydrated
Cold weather often reduces our ability to recognize that we are becoming dehydrated. If you are thirsty you have already become dehydrated. Try putting warm or hot water in a water bottle so that your water doesn’t freeze when training for extended amounts of time outside.
Take Action
If someone is suffering from a cold-related illness, get him or her into a warm location as soon as possible. Identify a nearby warming location before the start of training or play.
During games provide blankets or other items for players to stay warm while they are on the bench and allow additional substitutions or warming breaks.
Step One - Determine Wind Chill Temperature
The effects of cold weather can impact health and safety during practices and games. The definition of “cold stress” varies across the United States, depending on how accustomed people are to cold weather. A player from Minnesota will have a much different threshold for cold than a player from Florida.
NOTE: This table was adapted from the NOAA and NWS. It is compiled from the following formula Wind Chill (ºF)= 35.74 + 0.6215T - 35.75(Vˆ0.16) + 0.4275T(Vˆ0.16) where, T= Air Temperature and V=Wind Speed (mph).
Step Two - Find Your Alert Level
Use this chart to determine the alert level at your location based on the wind chill temperature.
* In wet environments with colder conditions, the following situations are accelerated. Use additional caution to recognize potential cold injuries. (NOTE: These WCT guidelines were adapted from the NATA position statement: Environmental Cold Injuries by Cappaert et al. 2008.)
COMMON COLD RELATED ILLNESSES
HYPOTHERMIA
Hypothermia is the result of your internal body temperature dropping to 95 degrees Fahrenheit (35 degrees Celsius) or less. It can be fatal if not detected promptly and treated properly.
Hypothermia typically begins with feelings of intense cold, shivering and behavior which are more quiet and disengaged than normal. As the condition worsens, the individual seems confused, sleepy and may begin slurring speech. To begin treating hypothermia, start by warming the center of the individual’s body first. Make sure they are dry and cover them with layers of blankets, clothing, towels or whatever else is around to contain their body heat. Warm nonalcoholic beverages may also help increase body temperature. If hypothermia is suspected, get the on-site medical provider or call 911.
Recognize
- Shivering vigorously or suddenly not shivering
- Increased blood pressure
- Lethargy
- Impaired mental function
- Slurred speech
Recover
- Remove damp/wet clothing
- Apply heat to the trunk of the body, not limbs
- Provide warm fluids and food
- Avoid applying friction massage to tissues
WARNING:
Do not use a hot shower or bath to treat hypothermia because it could cause the individual to go into shock.
*If symptoms persist seek medical attention from a physician or Emergency department.
FROSTBITE
Frostbite is what happens when skin and tissue actually begins freezing. It can cause numbness, tingling or stinging in the affected area. The skin may also lose its natural color, turning pale or bluish. Frostbite can permanently damage body tissue, leading to the loss of an extremity in severe cases.
The most commonly affected areas for frostbite include: nose, ears, cheeks, chin, fingers and toes. Use body heat or warm (but not hot) water to begin warming the affected area.
Recognize
- Swelling/Edema
- Redness or mottled gray skin appearance
- Tingling or burning
- Blisters
- Numbness or loss of sensation
Recover
- Gradually rewarm affected area with warm water
WARNING:
- Do not rub or massage the frostbitten area. This may actually increase the damage.
- Do not use heating pads, heat lamps or the heat of a stove, fireplace, or radiator for warming since affected areas are numb and can be easily burned
*If any of the symptoms persist for longer than a few hours, seek medical attention from emergency department or physician.

Lightning & Severe Weather
Lightning & Severe Weather
Lightning is one of the top ten causes of sudden death in sport.1 As the majority of soccer is played outdoors, lightning and severe weather pose a threat to player health and safety. U.S. Soccer’s Recognize to Recover program, with the help of the Korey Stringer Institute, provides these guidelines for responding quickly and safely when lightning and severe weather threaten practice or a game. When it comes to making decisions to suspend or cancel play due to weather condition, coaches, officials, athletic trainers and administrators all share responsibility. These same individuals should be aware of close safe shelter locations and know how to evaluate when it is safe to resume play after severe weather leaves an area.
1. Casa DJ, Guskiewicz KM, Anderson SA, et al. National Athletic Trainers’ Association Position Statement: Preventing Sudden Death in Sports. J Athl Train. 2012;47(1):96-118.
RECOVER
If someone is injured by a lightning strike, follow these emergency management steps:
- Call 911 and alert emergency medical responders (EMS).
- Establish that the area is safe before moving to help victim. If there is more than one victim, first assist those who appear in the most severe condition.
- Move individual(s) carefully to a safe location (victims of lightning strikes are safe to touch and do not carry an electric charge).
- Initiate CPR on victims who are unconscious, not breathing or have no pulse. Use an automated external defibrillator (AED) if one is available.
- Evaluate the individual(s) for additional injuries, such as broken bones or dislocations. Notify EMS of the potential injuries when they arrive on the scene.
Under no circumstances should a player injured in a lightning strike return to the game or practice. Injured players should only be allowed to return to play after a thorough examination and release by a qualified physician.
RECOGNIZE
- No place outside is safe when thunderstorms are in the area. All activity should be suspended, even if lightning or thunder has not yet been observed, and everyone should get indoors. Communicate this information completely and quickly to all participants.
- Consult the National Weather Service, the Storm Prediction Center or local media outlets for severe weather watches and warnings. Alerts can even be sent directly to your mobile device while you are on the field.
- Safe locations should be available with enough capacity to hold all who may need safe shelter. A primary location would be a fully enclosed building with wiring and plumbing. A fully enclosed vehicle with a solid metal roof, like a school bus, would be a safe secondary option. Open fields and open-sided shelters are not safe. If there are no adequate safe shelters close to the field, play must be stopped well in advance of the storm to allow everyone to travel to a safe place or their home.
- If it’s been half an hour since thunder, it’s safe to go outdoors. Outdoor activity may resume 30 minutes after the last sound of thunder or flash of lightning. The 30-minute clock restarts every time lightning flashes or thunder sounds.
Warning signs of a lightning strike:
- Feeling the hair stand on end
- Skin tingling
- Hearing crackling noises
If these occur, assume the lightning safe position:
- Crouch on the ground as low as you can
- Put all your weight on the balls of your feet
- Keep your feet together
- Lower head and cover your ears
- Do not lie flat on the ground

Field Conditions
Field Conditions
Field conditions vary from location to location, but safety practices are the same. There may be hazards on the field that need attention before safe play can begin.
RECOVER
- If hazards remain, play should be suspended or moved to a different location.
- Know your goal: There are 500,000 soccer goals across the United States in many shapes and sizes, each with specific safe anchoring guidelines. Anchor your goal correctly.
RECOGNIZE
- Trash and debris, including rocks, should be removed from the field.
- Make players aware of inconsistent surface conditions, such as uneven edges or bumps.
- Soccer goals should be properly anchored with weights or posts to prevent tipping forward.

CDC Resources for Healthy Travel
CDC Resources for Healthy Travel
Millions of U.S. residents travel internationally each year (more than 68.2 million trips in 2014!). We travel for a variety of reasons – for work, for relaxation, to visit friends and relatives, and to explore new cultures. As a U.S. Soccer player, coach, family member or referee, you may find yourself traveling overseas for a match or tournament. While an illness or injury could ruin anyone’s trip abroad, for you it may mean the difference between a win and a loss.
The Centers for Disease Control and Prevention (CDC) provides up-to-date recommendations for safe and healthy international travel. CDC also provides important country-specific health information, including the latest notices on events and outbreaks happening around the world.
You can use the Travelers’ Health page on the CDC website as a go-to resource:
- Access health recommendations for your travel destination(s), including vaccines and medicines you may need
- Find a healthcare provider in the U.S. specializing in travel medicine
- Learn more about travel health topics
- Download free mobile apps to help you plan for a healthy trip
For more information, visit CDC Travelers’ Health.
View the CDC's current list of worldwide health notices.